Services
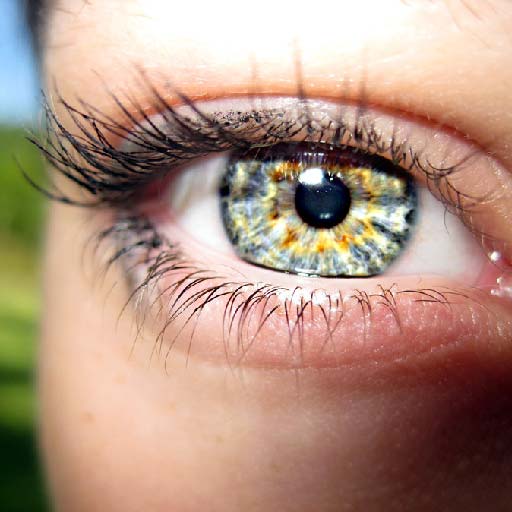
Optical Department
There are numerous choices when deciding on prescription glasses or contacts. Glasses not only need to look great, they need to fit your facial characteristics and lifestyle. From the workout room to the board room, we have an amazing selection of high quality eyewear to choose from, and a team of dedicated professionals who can assist you in making the right selection. There are also plenty of choices when selecting contact lenses, each offering different advantages over another. Let our trained professionals direct you towards the perfect choice for contacts that will fit both your personal eye characteristics and lifestyle.

Glasses
When you first look into a mirror, what do you see? Your face! Because glasses play such an important roll in defining your individual style, it’s important the glasses you choose will compliment your facial characteristics, lifestyle and, of course, look great. So while choosing the perfect pair of glasses can be a daunting task, it doesn’t have to be. Let our trained professionals guide you towards the perfect pair of glasses for your personality, lifestyle, and your budget. We offer a full spectrum of eyewear from many of today’s top designers, so you can be sure to find plenty of great style choices. Our dedicated professionals are ready to help you find the perfect look, and perfect fit.

Contact Lenses
Contact Lenses are a great alternative or complement to glasses for those who require corrective eyewear. They come in a variety of forms, made of different materials, and designed for different patterns of wear. Our specialists can help choose the best type for your eyes, furnish you with the correct prescription, and provide expert instruction for proper care and use of your contacts.
General Eye Examination
Eye exams are an important part of maintaining good overall eye health. Having regular eye exams is a critical component in detecting eye diseases or problems in their early stages when they are often still treatable. With regular eye exams the doctor can sometimes detect a problem before any noticeable symptoms begin to occur. Eye exams are necessary to prescribe proper corrective lenses or contacts, but can also serve a more specialized purpose, such as determining eligibility for laser refractive surgery, or monitoring an eye condition. Regular eye exams are the key to preserving good vision for life.
A thorough eye examination consists of a variety of standard tests designed to measure visual acuity and other vision faculties, as well as observe the health of the eye and check for common eye diseases. There is no pain or discomfort associated with an exam, and they typically take less than an hour.
General eye exams can diagnose a variety of eye conditions early on and are the best way to preserve good vision. For children, strabismus (crossed eye) and amblyopia (lazy eye) can often be diagnosed and treated in early childhood, avoiding life-long vision impairment. Also, rare eye conditions from birth (like congenital cataracts) can be diagnosed and treated. For all ages, refraction tests can determine whether prescription eyewear would be beneficial, and what power is necessary. Furthermore, many debilitating eye diseases can be diagnosed before noticeable symptoms occur, potentially making the difference between minor damage and major vision loss.
Eye exams are recommended regularly throughout all phases of one’s life. In the first three years, infants should have their vision checked as part of regular pediatric checkups. Between age three and six, an eye exam every year or two is recommended. Throughout childhood and the teenage years, exams should be scheduled as necessary. Exams are recommended for seniors every one to two years. People with diabetes should have at least one exam per year. Exams are also more frequent for patients monitoring a diagnosed eye condition, or with a hereditary predisposition to an eye disease.
Introductory interview
The doctor will ask basic questions about a patient’s medical history and eye health history.
External examination
The doctor inspects all outward visible parts of the eye and surrounding tissue.
Pupil inspection
The patient’s pupils will be inspected for equal size and regular shape. Then the doctor tests how they react to light and objects at various distances.
Eye muscle health and mobility
Eye movement is checked in six directions (corresponding to the six extraocular muscles), as well as tracking a moving object (such as a pen).
Visual field
The patient covers one eye at a time, and with the other eye gazing straight ahead, identifies objects in peripheral vision (often simply the number of fingers the doctor is showing.)
Visual acuity
A common means of measuring visual acuity is the Snellen chart. This is a large card or projection with progressively smaller horizontal lines of random block letters. The test determines how well a patient can discern detail at a given distance. Patients taking this test will cover one eye and then read aloud the letters of each row, starting from the top. The smallest row that can be accurately read indicates the patient’s visual acuity in that eye.
Refraction
This test is used to find the best corrected vision, if necessary for prescription eyewear or contacts. The doctor will try various lenses in front of each eye, as the patient focuses on a chart at a distance or up-close, to help determine the best power of correction.
Color vision
The doctor shows the patient a series of images with symbols embedded in color dots or patterns. Based upon the patient’s ability to identify the symbols, certain types of colorblindness can be diagnosed or ruled out.
Ophthalmoscopy
This test is often done with an ophthalmoscope, a handheld instrument with light and magnifying lenses. Alternatively, the doctor may use other means, such as a slit lamp, which affords a more three-dimensional view. Ophthalmoscopy aims to inspect the retina and surrounding internal eye. This test can help diagnose problems with the retina or detachment of the retina, and monitor diseases like glaucoma and diabetes. An opacity in the eye can indicate a cataract. Sometimes the doctor will dilate the pupils with eye drops, to gain a wider view of the internal eye.
Tonometry
This test measures intraocular pressure, which can be a sign of glaucoma if pressure is abnormally high. Internal eye pressure is measured either with a puff of air at the cornea or brief direct contact with the cornea, to measure how easily it is pushed inward.
Conditions & Treatments
The eyes are our windows to the world. When good vision is threatened by a disease or other eye condition, it is important to consult an optometrist for treatment as early as possible. In almost every case, early detection and treatment is the key to preserving good eyesight throughout life. We provide complete eye care and treatment for many common and not-so-common eye conditions.
1. Amblyopia (lazy eye)
An eye condition which develops in early childhood. For a number of reasons, the images from one eye (or in rare cases, both eyes) will be “ignored” by the brain. If this is left untreated, especially during the early vision development period in one’s life (until around age nine), these neurological pathways will become permanent, resulting in a lifetime of reduced vision. Having one amblyopic eye also puts added strain on the dominant eye, in which case future eye disorders are more likely.
Amblyopia symptoms may include:
- Squinting or closing one eye to see things.
- Poor depth perception and contrast perception.
- Poor visual acuity in general.
Amblyopia is often difficult to diagnose in children, since they often don’t know they have a vision problem. A doctor usually tests for the condition by blocking each eye and observing the patient’s response to visual tests. Amblyopic patients will often tend to do poorly on three-dimensional image tests.
Several conditions lead to Amblyopia:
- Strabismus (crossed eye) A condition where the eyes are misaligned, and do not gaze at exactly the same target. A child’s brain will adapt, and learn to ignore the image from the crooked eye, to prevent double vision. Surgery may be necessary to treat the strabismus, but the weak eye must also be treated for amblyopia.
- Refractive discrepancy In this case the eyes have markedly different levels of nearsightedness, farsightedness or astigmatism. The blurrier eye is ignored by the brain. Once diagnosed, this vision condition may be treated with corrective lenses; however, often the amblyopia must be treated as well.
- Eye clouding or obstruction Other eye problems such as trauma, congenital cataract, scarring, or anything preventing a clear image can result in disuse of that eye. The ophthalmologist must address the obstruction, often by surgery, and then treat the amblyopia.
Treatment
Whatever the origin, treating amblyopia requires a therapy aimed at making the child use the weak eye. Most commonly used is an eye patch over the dominant eye worn full time or intermittently, over a period of a week or two, or longer, until the weaker eye matches the stronger one. Alternately, the optometrist may prescribe a blurred lens, or Atropine eye drops, which prevent the dominant eye from focusing. These serve the similar purpose of imposing use of the weak eye.
Proper treatment during early childhood will often lessen or reverse amblyopia; however, it is common for the disorder to recur during this period requiring treatment to resume. Once a child passes the age of nine, amblyopia will usually not relapse if it has been successfully treated up to that point. Conversely, it is much more difficult to treat older patients with amblyopia. Nonetheless, treatment can still be worthwhile for those beyond early childhood.
If your child is experiencing any symptoms of amblyopia, we encourage you to contact us today to schedule a consultation.
2. Cataract Care
A cataract is an opacity that clouds the natural lens inside the eye. Normally the path of light to the retina (where the light sensors are) is as clear as possible. When proteins that make up the lens clump together, the resulting cataract blocks some of the light, making vision blurry or hazy.
Cataracts typically occur more frequently in the aging population, however there are many other factors such as family history, diabetes, long term UV exposure, or certain medications like steroids that can cause cataracts. Also, previous eye injuries can be an attributing factor.
Cataract symptoms may include:
- Blurry vision.
- Lights seem too bright or have a “halo” effect.
- Double vision in one eye.
- Decreased night vision – sensitivity to glare from headlights.
- Dull or fading colors.
Some people actually experience an improvement in their near vision during the beginning stages of a cataract. Unfortunately, this effect goes away as the disease progresses. Early on, a cataract may be treated with increased glasses or contact prescription. Once the cataract begins to interfere with daily tasks such as reading and driving, surgery is the only remaining option.
Cataract Surgery
Cataract surgery is a very common procedure, and complications (if any) are rare and treatable. The surgery itself is highly successful in improving the vision of patients about 95% of the time. Cataract surgery is an outpatient procedure usually taking less than 30 minutes to complete.
During the surgery, the doctor removes the cloudy natural lens from the eye while the patient is under a topical anesthesia. Next, the doctor inserts an intraocular lens (IOL), which remains permanently in place of the removed natural lens. The IOL compensates for the magnification the old lens provided. Modern IOLs are designed for various functions and made out of different materials; your doctor will know which is most appropriate for your individual case. After the operation the doctor will apply a shield for the eye and provide you with eye drops to use as directed.
Recovery from Cataract Surgery
The patient may return home the day of the procedure. With proper rest and avoidance of any strenuous activities such as heavy lifting, recovery is usually a matter of days, with only minor discomfort. Several follow up appointments will be required to ensure the eye is healing properly and initial results are sustained.
If you are experiencing any symptoms of cataract problems, we encourage you to contact us today to schedule a consultation.
3. Dry Eye
Dry eye syndrome is a common disease in which the eye under-produces tears or tears leave the eye too quickly. A normal functioning eye constantly produces tears to form a tear film, which acts as moisturizer and lubricant. For someone with dry eye, the resulting lack of moisture and lubrication can cause a variety of problems.
Dry eye symptoms may include:
- A burning, stinging, or scratchy sensation in the eyes.
- Eyes may redden and become easily irritated by wind or smoke.
- The eyes may produce stringy mucus.
- Contact lenses may be difficult or impossible to wear.
- Sometimes the eye will actually produce excessive tears, and overflow.*
*Though it sounds contradictory, sometimes the eye will actually produce excessive tears, and overflow. The eye becomes irritated by the lack of lubrication and attempts to cleanse itself with a flood of tears. This is a similar phenomenon to the tearing that occurs when foreign matter is stuck in one’s eye.
Dry eye syndrome is typically more common in older people and women; however, there are many other factors that can cause this to happen. A common cause of dry eye can be over the counter and prescription medications such as antihistamines, beta-blockers, sleeping pills, pain relievers and many others. Overuse of diuretics can also play a role in developing dry eye. For this reason, it is very important to inform your optometrist about any medications you are currently taking, which can help the doctor in the proper diagnosis of the disease.
Sometimes the cause is unknown in a case of dry eye. Known causes of dry eye may be natural, related to a larger condition, or the side effect of certain medications. Also, tear production often slows down as people get older. This is particularly common for women after menopause.
Treatments for dry eye:
- Artificial tears Mild to moderate cases of dry eye syndrome may be treated by applying artificial tear eye drops as little or as often as necessary. There are a wide range of products available without a prescription that the doctor can recommend.
- Prescription medications Can sometimes increase tear production for those with chronic dry eye. It does this by targeting inflammation in the eye.
- Conserving tears An effective way to make better use of the tears in the eye is surgery to close the tear ducts, thus preventing existing tears from leaving the eye as quickly. This may be done temporarily, with punctal plugs made of collagen, or permanently with silicone plugs or by cauterizing the tear ducts closed.
- Controlling one’s environment Patients should avoid situations in which tears evaporate quickly; for example, by using a humidifier in a dry house, wearing wrap-around glasses in the wind, and not smoking.
If you are experiencing any symptoms of dry eye, we encourage you to contact us today to schedule a consultation.
4. Glaucoma
Glaucoma is a disease that affects the optic nerve, the part of the eye which receives images collected by the retina and sends them to the brain. Every eye maintains a certain amount of internal pressure, called intraocular pressure. When this pressure rises to abnormal levels however, it can put extra stress on the optic nerve, causing significant damage. Optic nerve damage results in loss of vision, and ultimately blindness.
The front of the eye is constantly producing a fluid called aqueous humor. A healthy eye will continually produce small amounts of aqueous humor to ensure consistent pressure within the eye. When normal drainage becomes slowed or blocked, pressure increases, and may lead to glaucoma. There are several different types of glaucoma the two most common types being chronic open-angle glaucoma and closed-angle glaucoma.
Chronic open-angle glaucoma is the most common form of the disease and usually develops with age. With this type of glaucoma, pressure gradually increases around the eye causing it to work less effectively over a period of time. There are no symptoms in the early stages of open-angle glaucoma. Peripheral vision is usually the first to deteriorate. As the disease becomes more advanced, blank spots begin to appear in one’s vision. If left untreated, it eventually develops to blindness. The best way to avoid serious vision loss is early diagnosis and treatment.
Risk factors for chronic open-angle glaucoma include:
- Advanced age.
- Family history of the disease.
- Higher-than-normal intraocular pressure.
- Certain ethnic races, particularly those of African descent.
- Certain diseases or conditions, especially diabetes, farsightedness or nearsightedness, or previous eye trauma or surgery.
Closed-angle glaucoma is less prevalent, but is considered a real eye emergency. This type of glaucoma occurs when a patient’s pupil moves or dilates and actually blocks off the drainage angles in the eye. This is considered a medical emergency in which an ophthalmologist should be contacted immediately to avoid any loss of vision.
Symptoms of closed-angle glaucoma include:
- Severe eye pain.
- Headache.
- Blurred vision.
- Nausea or vomiting.
- Rainbow halos around lights.
High risk factors for closed-angle glaucoma include:
- Extreme farsightedness.
- An iris that is abnormally large or far back in the eye.
- Advanced age.
- Heredity.
- Certain ethnic races, especially Asians.
Treatments for glaucoma:
There are a wide range of treatments for the disease, including medication, laser surgery and traditional surgery. The treatment (or combination of treatments) for an individual is chosen based upon the type of glaucoma and other details of the particular case. One option is medication such as prescription eye drops which help to reduce intraocular pressure, or pills called carbonic anhydrase inhibitors which slow down fluid production within the eye.
Laser surgery has also become a common treatment option for glaucoma. For open-angle glaucoma the doctor may choose a trabeculoplasty, a painless laser procedure which uses light to shrink and stretch eye tissue to allow more drainage of fluid. For closed-angle cases, in which the iris is blocking drainage of aqueous humor, a laser surgery called iridotomy may be preformed.
Other glaucoma treatment options involve various traditional surgeries. A common surgery for open-angle glaucoma is the trabeculectomy, where a doctor creates a small flap in the sclera (white part of the eye). Underneath the surface of the sclera, the doctor creates a small reservoir, called a filtration bleb, into which aqueous fluid may drain and then be disbursed, further reducing intraocular pressure.
There are a number of treatments available for Glaucoma patients. If diagnosed with glaucoma, your ophthalmologist will consult with you on your options in order to maintain the best possible health of your eyes.
If you are experiencing any symptoms of glaucoma, we encourage you to contact us today to schedule a consultation.
5. Macular Degeneration
Macular degeneration affects cells in the macula, which is the part of the retina responsible for central vision. Central vision is essential for most basic tasks like reading, driving, recognizing people, etc. Thus, although macular degeneration leaves peripheral vision un-impaired, it can be quite debilitating in its advanced state.
The disease exists in two forms, dry and wet. Dry macular degeneration is by far the most common (roughly 90% of all cases). However, it is the milder of the two forms, develops gradually, and usually leads to only minor vision loss. Dry macular degeneration tends to occur when yellow fatty particles called drusen accumulate in the retina underneath the macula. This build-up results in thinning and drying-out of the macular cells.
Wet macular degeneration is less common, but the vast majority of severe vision loss cases result from this form. First, abnormal blood vessels form underneath the surface of the retina. Leakage of blood and other fluids from these blood vessels permanently damage the outside cells (which detect incoming light). As these cells are damaged, vision is lost.
The primary cause of macular degeneration remains unknown. Macular degeneration typically occurs more frequently in the aging population with patients over 60. Research has shown there are many other factors such as family history, smoking, hypertension, obesity, and/or a high cholesterol, high fat diet that may contribute towards the development of macular degeneration.
Macular degeneration symptoms may include:
- Shadows, blurriness, or holes in the center of vision.
- Straight lines appear wavy.
- Trouble seeing details both up close and at a distance.
- Difficulty telling colors apart, especially ones close in hue.
- Vision can be slow to come back after bright light exposure.
Treatment for dry macular degeneration:
Unfortunately, there is no treatment for the dry form of macular degeneration. Those at high risk should schedule a checkup with their optometrist at least once every one to two years, to catch the disease in its infancy. Also, it is thought that dietary supplementation of antioxidants and zinc may help to slow its development.
There is also no cure for wet macular degeneration. There are, however, several treatments designed to combat the disease. Early detection is very important because once vision is lost there is no treatment to regain it.
Treatments for wet macular degeneration:
- Laser photocoagulation Seals abnormal blood vessels with a heated laser. This treatment will sometimes halt the disease, thus saving the remaining vision of a patient. However, the laser leaves a scar, creating a permanent blind spot in the patient’s vision. The treatment is only applicable to a small segment of cases, in which some vision is sacrificed to save remaining vision.
- Photodynamic therapy Employs a light-activated drug and a “cold” laser. The drug is injected intravenously. Then the doctor shines the laser on the affected area, which activates the drug in the targeted tissue and blocks the leaking blood vessels. This procedure leaves no scar, and may be repeated several times as necessary.
- Anti-angiogenesis drugs These inhibit proteins which contribute to abnormal blood vessel growth. They are known as anti-VEGF (anti-vascular endothelial growth factor) drugs. There are a variety of drugs that can be applicable for this purpose, some FDA approved, and some off-label (officially approved for a different application).
- Other pharmaceutical treatments For example, angiostatic treatments, which combat blood vessel growth with steroid injections.
If you are experiencing any symptoms of macular degeneration, we encourage you to contact us today to schedule a consultation.
Laser Refractive Surgery
Laser refractive surgery has seen a significant increase in popularity over the past decade. This popular procedure is done as a corrective measure for those suffering from nearsightedness, farsightedness and astigmatism. Millions of these procedures have been performed throughout the country with an overwhelming rate of satisfaction.
LASIK Eligibility Evaluation Do you suffer from nearsightedness, farsightedness, or astigmatism? Do you find glasses or contacts cumbersome or uncomfortable, and wish you could reduce their prescription or discard them?
If you answered “YES” to either of these questions, you may be a good candidate for LASIK or other vision corrective surgery. Before the decision can be made however, you must have an eligibility exam and consultation. The doctor will ask questions about your medical history and give a thorough eye exam designed to determine if the procedure is appropriate for your individual case. The doctor will also talk about the benefits, risks, available options, and preparation and recovery associated with the surgery to ensure that your goals and expectations are realistic.
If you wish to be free from glasses or contacts, or just want to greatly improve your vision, corrective laser eye surgery could be the solution. There are many different types of laser surgeries offered today. Consult with your doctor on which option is best for you.
1. LASEK (laser epithelial keratomileusis)
A relatively new type of corrective laser eye surgery. It employs an alcohol solution to loosen the very outer layer (epithelium) of the cornea. Once the laser correction has been performed, this epithelial flap is replaced as a sort of natural bandage. LASEK is a good alternative for those patients who are not candidates for LASIK surgery due to thin corneas.
Reasons to consider LASEK:
- Wish to reduce or eliminate dependence on glasses or contacts for those with myopia, hyperopia or astigmatism.
- The epithelial layer is kept, reducing healing time and pain compared to PRK.
- An alternative for patients with thin corneas who are not candidates for LASIK.
- Reduces the chances of post-operative corneal haze, compared to PRK.
- Patients experience dry-eye less often after LASEK than compared to LASIK.
The Procedure
For the LASEK procedure, first the doctor creates an epithelial flap. Alcohol is used for about 30 seconds to loosen the epithelial cells. Then the epithelium is lifted, with the help of a trephine blade, and folded aside, to allow access to the inner layers of the cornea. At this point, the excimer laser ablates (burns off) the carefully mapped tissue, just as in LASIK and PRK. After the laser correction is complete, the doctor replaces the epithelial flap, and applies a bandage contact lens to aid in healing.
The Recovery
The epithelial layer fully heals in about a day, though usually the patient must wear the bandage contact lens for about four days. Patients may experience mild discomfort, irritation or pain for the first couple of days after the procedure. The doctor will schedule several check-up appointments to monitor the healing process, followed by periodic visits over the next several months. During the recovery process, the patient should rest and refrain from any strenuous activities for at least a week. Most patients can return to work in a few days, though it is best to take off whatever time needed to ensure a smooth recovery.
2. LASIK (laser assisted in-situ keratomileusis)
The most commonly performed and well known vision correction surgery. Using an excimer laser, the doctor re-shapes the cornea (the stationary refractive element at the front of the eye) so that images are focused to the correct spot on the retina (the light receptor of the eye). The success rate with this procedure is excellent, with most patients achieving 20/20 vision or better upon completion.
The LASIK procedure itself involves little or no discomfort (or pain) both during the procedure and through the recovery process. Also, eyesight improvement is almost immediate, and maximum vision is typically achieved within a few days.
Reasons to consider LASIK:
- Nearsightedness (myopia).
- Farsightedness (hyperopia).
- Astigmatism (irregularly shaped cornea).
- Desire to decrease or eliminate dependence on glasses or contacts.
The Procedure
During the procedure, the doctor first administers a local anesthetic via eye drops, so the patient will feel no pain during the surgery. A speculum is then placed over the eye to prevent the patient from blinking. Next, the surgeon cuts an extremely thin flap from the outer layer of the cornea, using a microkeratome (a small blade specially designed for this purpose). The flap is folded to the side, and the excimer laser, programmed with the individual map of the patient’s eye, removes excess tissue with quick pulses of concentrated light. This process usually takes less than a minute. Once this is done, the doctor folds the flap back into place and surgery is complete.
The Recovery
The patient may go home shortly after the procedure; however, someone else must drive or alternate transportation must be arranged. Patients will be asked to get lots of rest, avoid any strenuous activities, and avoid rubbing the eye area for a period of time. There are follow up appointments with the doctor 24 to 48 hours after the procedure and periodically over the following weeks and months. Vision should dramatically improve in the first few days following surgery. The patient often may return to work in a day or two, though it is best to take a few days off to ensure a smooth recovery.
3. PRK (photorefractive keratectomy)
Was at one time the most common laser eye surgery. It uses the same excimer laser as the LASIK procedure to reshape the outer layer of the cornea to correct for nearsightedness, farsightedness, and astigmatism. These days LASIK is more common, but PRK is still an alternative for patients who cannot undergo LASIK Surgery.
Reasons to consider PRK
- Nearsightedness (myopia)
- Farsightedness (hyperopia
- Astigmatism (irregularly shaped cornea)
- Cornea too thin for LASIK
- Pupil too large for LASIK
The Procedure
In preparation for surgery, anesthetic eye drops are administered. Next, a speculum is placed in the eye to keep the eyelids open, which is normally not uncomfortable. While the patient fixes his or her gaze on a target, the laser reshapes the cornea by removing tissue (a process called ablation), which is controlled and closely monitored by the doctor. The laser is actually guided by a detailed map of the patient’s eye which has been programmed into a computer beforehand. The ablation usually takes around a minute for each eye, depending on how high the patient’s vision prescription is. Most patients feel no pain during the procedure. After the procedure is complete, a bandage contact lens is placed on the eye. The patient may go home shortly after the procedure; however, someone else must drive or alternate transportation must be arranged.
The Recovery
The doctor may prescribe pain medication for recovery; however, most patients don’t require it since only minor discomfort is experienced. The doctor will also schedule several check-up appointments to monitor the healing process, followed by periodic visits over the next several months. During the recovery process, the patient should rest, and refrain from any strenuous activities for at least a week. Most patients can return to work in a day or two, though it is best to take a few days off to ensure a smooth recovery.
